This page is dedicated to show some examples of Navicular lesions and how I have applied mechanical changes to unload the areas of pain. I see many cases that have lameness that blocks to a low palmar digital nerve block and have many different foot types. Many structures are anesthetized with that nerve block and it is up to the practictioner to decide based on hoof characteristics, radiographic changes and soft tissue parameters what the most likely area of disease exist. However many times several structures are involved and without an mri it may be difficult to completely ascertain a definitive structure or set of structures involved.
Most cases in my practice do not get the luxury of an mri and we must spend our efforts in therapy that will aid in recovery based on unloading the painful region in the heel region. Learning to evaluate the lower limb mechanics and soft tissue parameters is paramount in deciding a therapeutic shoeing approach. For example, think of a case that has a negative palmar angle, upright pasterns, low bone angle, long toe lever, 5mm of sole depth below medial palmar wing and poor quality wall mass. This case can be bilateral or opposite a higher grade club and will also often be hoof tester responsive and block to a low palmar digital block. These parameters suggest a very unhealthy, beat up heel and may or may not have true navicular bone lesions.
If you add navicular lesions and poor quality hoof it makes it more difficult to manage long term. I see many cases that have been diagnosed as navicular based on hoof tester and block but merely have run out of foot and have very sore bruised tissue in the palmar aspect of the hoof. These respond nicely to increased self adjusting palmar angle to align digits, a greatly reduced toe lever and a positive pressure frog plate to incorporate the entire buttress for load bearing. I feel that with proper digital alignment loads are directed along a line parallel to the axis of the first phalanx (long pastern bone) unloading the painful heel with load transferred more to middle of foot. Once sole depth and foot mass has recovered the patient is much more comfortable and less and less mechanics are needed to maintain proper digital alignment. These cases will have minimal response to coffin joint and navicular bursa injections.
The second type of situation I see is a good foot that holds a positive palmar angle, good sole depth and typically has a stronger bone angle. This group will often be bilateral lame or more lame in the club (higher profile heel) foot, have a shortened, choppy, stabbing gait and blocks to a low palmar digital nerve block. These are often also responsive to hoof testers across frog and trot off more lame if placed on a toe wedge for 1-2 minutes. These cases can have large radiographable navicular lesions or barely any at all. This group represents a more likely true navicular bone disease.
Many mild cases respond to bute and rest. Many cases respond to coffin joint joint injections alone but if one does not respect the mechanical aspect of the syndrome the response will be short lived. A common therapy is navicular bursa injections in which a needle is placed through the deep digital flexor tendon into the navicular bursa which lies between the navicular bone and flexor tendon. I personally do not perform these in my practice as I do not like the fact I am penetrating the tendon with each injection and I have such profound results with mechanics alone or in combination with coffin joint injections with hyaluronic acid and triamcinolone (cortisone).
Understanding the anatomy and lower limb mechanics allows one to design a therapuetic shoe that will unload the painful interaction between the navicular bone, flexor tendon and supporting ligaments of the navicular bone. A recent study states that for every one degree change in palmar angle the load that the flexor tendon exerts on the navicular bone is changed by 4%. With that understanding altering a severe, painful case with a 3 degree wedge offers only 12% reduction in load and minimal improvement. The level of mechanics must equal the level of damage/pain. If higher mechanics are required then a period of rest for 6-8 weeks with hand walking only and bute for 3-5 days to decrease pain and inflammation. Once we have unloaded the painful areas it now has the change to heal to some degree and much of the inflammation will subside. Reducing the level of mechanics (rocker/type of shoe) over 2-3 cycles is often possible. Many cases will maintainable in a rockered full rocker shoe or rockered conventional shoe depending on degree of bone/tendon damage. This is an effective tool for maintenance of lesions in this area. Clients often ask when can we go back to a flat shoe. These lesions are not going anywhere and as soon as you drop the palmar angle and engage the flexor/navicular bone interface pain will be evident.
Evaluation of the navicular bone involves a direct detailed radiographic approach with regards to generator setting and beam orientation.
I do not "nerve" (cutting of the palmar digital nerves) as I feel I have had success managing cases with shoeing mechanics. The nerving procedure leaves the horse without feeling of the foot and shoeing and walking around in the pasture becomes very high risk. A hot nail or puncture wound could go unnoticed until a raging infection is noted.
Learning this approach from Dr. Ric Redden has allowed me to help many horses that fail conventional therapies with shock wave, egg bars, heart bars, wedge pads, coffin joint injections, navicular bursa injections and tildren. Many of the cases that I see have had every other shoeing application by very competent farriers and are still are lame. A detailed evaluation of the level of disease present and application of a therapeutic shoe that supplies the necessary relief. Much more is available than many owners are aware with regards to new innovative techniques in therapeutic shoeing.
Below are some cases that I manage with shoeing mechanics.
 |
| A. Corresponding irregular flexor cortex radiolucenies (darker areas, loss of bone) |
 |
| Pre shoe radiogaph. |
 |
| Post shoe rads |
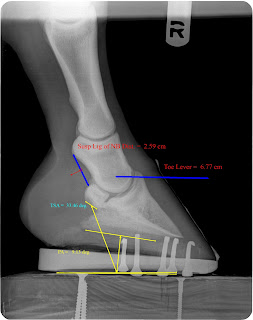
Notice reduction in toe lever, digital breakover and distance of origin to insertion of suspensory ligament of the navicular bone. Increased palmar angle represents the decreased amount of deep digital flexor tension and the increased tendon surface angle lessens the angle at which the flexor has to make as it courses to its insertion on the semilunar crest of the coffin bone. Remember that the tendon attaches to its muscle belly above the carpus (knee) and then attaches to the back of the coffin bone in the foot.
 |
| 3 large radiolucent (cyst/dark holes) at A. At B. a lipping noted at insertion of the supensory ligament of the navicular bone. |
 |
| High Beam Dorso palmar view showing corresponding radiolucent areas at A. and a more pointed bone at insertion of the suspensory ligament of the navicular bone. |
 |
| Pre shoe farrier friendly radiograph |
 |
| Post shoe radiograph |
This case was severely painful and required high scale mechanics with 6 weeks hand walking only. After reset with similar mechanics light riding began and lameness grade dropped considerably. Patient is maintained with the mechanics below. If becomes painful we simply increase the amount of rocker to increase palmar angle and unload the painful region of the navicular bone.
 |
| This radiograph is several months later with greatly decreased mechanics required after a time to allow healing of painful are
The following is a case from this week. This is a 7 year old pleasure horse with a long term history of choppy gait and off and on head bob responsive to bute.
1/5 lame bilateral but 2/5 on left turn in a tight circle. Left front is a grade 1+ club and podiatry style films confirm healthy soft tissue parameters. My thought process is: With healthy sole depth and minimal remodelling of the apex of coffin bone on a club foot I want to next look at the navicular bone to evaluate for lesions. This case shows significant lesions in several views. This are most likely in the distal half of the flexor cortex of the navicular bone. I find these similar lesions in younger non lame patients but I do feel as they reach middle age they begin to create lameness. Dr. Redden feels that the navicular bone of the club foot does not recieve as much load from the tendon versus the lower profile foot and does not develop as strongly as the low foot. I am beginning to feel that these lesions are developmental and become more degenerative with age and use. If dissected out these lesions will be a slight depression in the flexor cortex with a roughened edge that likely causes some abrasiveness to the deep digital flexor tendon.
My treatment plan is to drastically increase palmar angel to reduce load on the painful area. This will allow some decrease in inflammation and likely a lower mechanical shoe in the future. I have also prescribed a 5 day course of bute to decrease pain and inflammation. I choose mechanical options first as it is a very low risk treatment and we can always resort to injections of the coffin joint and/or navicular bursa. However I find that most of my cases respond very well to mechanical enhancement alone. I will let you know about the response we obtain in this case.
Below are images of the navicular bone, pre and post shoe podiatry radiographs and digital photos of the patient.
Click here to shop Dr. Reddens products (shoes, ultimates and much much more) SHOP NANRIC
Note the better digital alignment the drastic change in palmar angle, tendon surface angle and reduced toe lever. This shoe changed PA by 12-14 degrees which will unload the tendons load on the navicular bone by 50 to 60 percent.
Thanks for looking.
|
This is a 9 year quarter horse gelding that has had lameness issues since he was 3-4 years old. He has never been used outside of light training. I feel this type of navicular bone disease must have a genetic component as lesions where noted at an early age. This horse responded early on to low level mechanics that included a four point style shoe with digital breakover at the tip of p3. It progressed to needing significant mechanical enhancement but did respond to the enhanced mechanics applied via a rockered 4 point rail shoe. The horse was 4/5 bilateral lame on front before shoeing and 1/5 immediately post shoeing. A significant improvement was noted after the below shoeing method. The horse was euthanized due severity of disease and dissection was performed to further evaluate the navicular bone and compare to the radiographs. You will see below the lucent lesions noted in the high beam dorsopalmar radiographs and the 65 dg dorsopalmar radiographs. These lesions are present on the flexor surface of the navicular bone in which interacts with the flexor tendon. Note the tissue protruding from the lesions. This is tendonious tissue that has grown into the tendon and anchors the tendon to the navicular bone. I can imagine that at lower palmar angle the attachment tugging at the navicular bone lesions is terribly painful. This also explains why an increase in palmar angle and reduced digital breakover that reduced leverage and tension on the DDFT is so very helpful in this situation.
Many medical therapies are used in treatment of navicular disease however without appropriate mechancial treatment many medical therapies only offer temporary relief. Bursa injections, coffin joint injections, isoxoprine and tildren are common treatments. But you can see that without mechanical therapy that offers appropriate physical relief it can be difficult to manage. Cases like this can be difficult to manage at a performance level long term with mechanics and medical therapies and all but impossible without mechanical therapy.
Note the lucent regions on the radiographs and the corresponding lesion below. The tendon has grown into the navicular bone secondary to years worth of the tendon rubbing against the roughened flexor surface of the navicular bone. This causes abrasions on the tendon that leads to the adhesions connecting it to the navicular bone.
 |
| Viewing from front of hoof with navicular bone flipped up to expose the flexor (back) surface of the navicular bone in which the tendon glides over then attaches to coffin bone. |
 |
| Note the two adhesions on flexor surface. These where cut away from tendon |
 |
| This drawing shows the DDFT in green and adhesions in red |
Below are pre- and post-shoeing radiographs. Note the drastic changes in palmar angle, tendon surface angle and distance of navicular bone to the condyle of proximal second phalanx (short pastern). In the rocker shoe the system is now a self adjusting mechanism with greatly decreased load on lesions and a greatly reduced leverage on the ddft. Again, this horse's lameness improved at least 80 percent with application of this shoe.

















Thank you for this information. Very helpful.
ReplyDelete